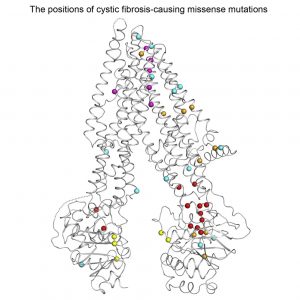
Molecular structure of the CFTR ion channel with circles marking positions of some disease-causing mutations (from Zhang and Chen, 2016).
As the most common fatal genetic disorder, cystic fibrosis (CF) has been at the forefront of genetic research since the gene responsible for it was discovered 40 years ago. But with more than 300 known disease-causing mutations, or variants of the CF gene, disease severity and treatment options can vary a great deal from one patient to another. Advances in stem cells and 3D culture systems could reveal new molecular insights about the disease and help find the right drug for each patient.
Most of us know CF as a lung disease, but it can affect other organs too. Its root cause is the body’s inability to move fluid through its inner tubes. And while this leads to the build-up of bacteria-trapping mucus in the lungs, it also affects the bile ducts’ ability to transport digestive juices from the liver and pancreas to the gut.
Caused by a mutation in a single gene called CFTR (Cystic fibrosis transmembrane conductance regulator), CF affects about 70,000 people worldwide, mostly of North European descent. One in 25 Canadians carry an abnormal copy of the gene, although both copies have to be defective for the disease to occur. In addition to 322 disease-causing variants, 1,700 more have been identified in patients, and they are either harmless, or of unknown consequence (the ramifications are explained here).
The CFTR protein is embedded into the lining of the body’s tubes where it allows ion flow across the cell surface to regulate fluid volume inside the tubes. Fine, hair-like structures, known as cilia, also cover the lining and their beating helps move the fluid to, for example, expel bacteria from the lungs and bring enzymes from the liver into the gut. Because CFTR mutations disrupt ion flow, this removes the fluid leaving cilia stuck in the resulting goo.
Christine Bear, Director of the Cystic Fibrosis Canada Program in Individualized Therapy (CFIT), at the Hospital for Sick Children in Toronto, is excited to be able to create lab-grown bile ducts and use them to learn more about the disease and even search for new treatments. For example, Bear hopes to better understand the role of cilia in CF. The cilia don’t just beat to move the fluid— they also sense signals from the fluid that feedback into the cell in a way that could affect CFTR function.
This interplay is not well known because fluid flow has been hard to study in the lab with standard methods. For a start, cells are typically cultured as a flat sheet covering the surface of the dish. This is clearly a very different geometry to the one they find themselves in inside the body’s tubes. But now it is possible to bioengineer tissue in a way that more closely mimics how it occurs in the body.
Through a Medicine by Design funded project, Bear teamed up with stem cell scientist Gordon Keller, of the University Health Network in Toronto, who was able to transform reprogrammed stem cells into cholangiocytes – specialized cells that line the bile ducts. These will be seeded inside tiny collagen tubes, manufactured by engineers on Axel Guenther’s team, at the University of Toronto. By passing fluid through these tubes, the researchers expect to be able to study for the first time how fluid composition and flow affect both the cilia and CFTR.
This may also allow them to search for drugs that can restore CFTR function. Working with CCRM, they are developing patient-derived tissue to study the effects of the CF variants seen among Canadian patients and for which there is no treatment.
So far, three drugs have been approved that work to increase CFTR ion conductivity, therefore targeting the cause of the disease and not just the symptoms. Though hailed as a breakthrough in precision medicine, these treatments come at a high cost yet their effects are modest and target only the most common CFTR mutations, leaving thousands of patients with more rare forms of the disease without treatment.
Researchers in the Netherlands have already tested drugs on balls of patient-derived gut tissue to see if this induces fluid intake and swelling as seen in tissue from healthy people. In a paper published last month, they reported success in matching 24 patients with rare CFTR mutations with effective treatment. And the same test had previously allowed the Dutch team to predict disease severity in newborn CF patients helping parents and physicians make decisions about therapy.
Of all the genetic disorders, CF has probably been studied the most but there is no cure yet. This is partly due to the diversity of CFTR variants among patients and it poses a real test for personalized medicine. Whether balls or tubes, 3D tissue culture grown with patients’ own cells could lend insight on individual forms of disease and point to the best treatment.
Jovana Drinjakovic
Latest posts by Jovana Drinjakovic (see all)
- Canadian immunotherapy holds promise for patients with brain cancer - September 9, 2020
- Could stem cells be enlisted to battle COVID-19? - March 26, 2020
- Study reveals large differences at the molecular level between stem cells grown on different biomaterials - April 18, 2019






Comments