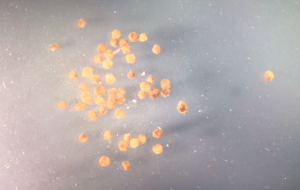
Click on the image to watch a video of a swarm of living robots swimming through water (time lapse). Credit: Douglas Blackiston and Sam Kriegman
“Regenerative medicine news under the microscope” is a new monthly feature highlighting big stories in stem cell research. I will sample the latest and greatest findings in recent press and package them into a single post.
This month, I am featuring more COVID-19 advances made through stem cell research, 3-week-old human-monkey embryo chimeras, the new NIH iPSC Neurodegenerative Disease Initiative, xenobots, and much more!
COVID-19: Intestinal implications
Though the virus has been with us for over a year now, scientists still have many questions about how COVID-19 infection affects human physiology. One burning question is how intestinal health may be influenced, given that gastrointestinal symptoms are sometimes observed in COVID-19 patients.
Modelling the colon and small intestine, human intestinal organoids can be infected in vitro and observed thereafter to determine whether or not SARS-CoV-2 has any adverse effects on the tissue. In doing this, Mithal et al. report that the virus is indeed able to infect intestinal cells. According to their research, the way in which the virus highjacks organoid cells results in ultrastructural changes – meaning rearrangements in cellular architecture so fine that an electron microscope must be used for visualization. This observation is consistent with previous characterizations in COVID-19 patients. An upregulation of inflammatory signatures were also recorded in epithelial cells.
A limitation acknowledged by the authors is that organoids often reflect fetal developmental time points in terms of their maturity; therefore, this must be kept in mind when attempting to draw conclusions about adult organisms. However, an interesting advantage offered by this intestinal organoid system is that it can be used to study different genetic susceptibilities to COVID-19, since not all patients exhibit gastrointestinal symptoms.
NIH’s iPSC Neurodegenerative Disease Initiative (iNDI)
The National Institutes of Health (NIH) is leading an initiative that will test upwards of 100 mutations associated with dementia, including Alzheimer’s disease, to better understand what exactly is causing brain cell damage in these patients and how all the dots connect. According to them, this will allow for the development of better therapies and preventative treatments. The way in which they’re trying to reach this goal is exciting: they’re calling it “the largest iPSC genome-engineering project to date.”
Led by Drs. Michael Ward and Mark Cookson, this project is unique in that each induced pluripotent stem cell (iPSC) line in use will have an identical genetic background, apart from one distinctive mutation previously linked to disease. This means that their goal of studying over 100 mutations will require the use of over 100 cell lines.
The cell lines will be made available to other labs as well, meaning that the entire research community will enjoy the benefits of this initiative.
The monkey-human chimera paper that everyone’s talking about
Moral conflict, excitement, anxiety, and many many questions (old and new) have been stirred up by a paper published in Cell this month – but you probably knew that already.
Tan et al. managed to generate chimeric embryos of human and macaque origins ex vivo using human extended pluripotent stem cells (hEPSCs). The hEPSCs differentiated into cell lineages reflecting peri- and post-implantation developmental time points, plus scRNAseq was used to shed some light on the developmental trajectories of the chimera-sourced cells. For 20 long days, these embryos survived in vitro conditions, marking a new milestone in chimera research.
However… the question is, why?
Some scientists believe that, one day, it will be possible to grow human organs in animals who will eventually act as donors to patients in need. This is a long way off, and is extremely complex in terms of the physiological, medical and ethical particulars. Dr. Paul Knoepfler has a fantastic, in-depth review of these issues on his blog. The long and short of it is: how human is too human when it comes to organ harvesting or other potential applications of these chimeras? Who will make these rules, and how will they be enforced? Are there alternative means to this end?
You won’t want to miss this read.
Aspiring to synthetic living machines: Xenobots
I must confess that this paper was published on March 31st but, by this date, my last blog was already written! I simply had to include this story here.
The name Xenobots stems from Xenopus laevis – the African clawed frogs whose stem cells were used in this study. Blackiston et al. obtained skin cells that had differentiated from frog embryos, and watched what happened as they proliferated and organized themselves into clusters outside of their usual niche. Instead of using their cilia to allow mucus to blanket the skin, the cilia were used for what appeared to be coordinated motility – and if you have any doubts about this, a midline formed wherein the cilia on one side of the epithelial ball would row to the left, and the other, to the right. They circle particles, do mazes without bumping into corners, and do not merge when they meet each other. In fact, they were found to respond to one another. Watch them go in the video (click on the image) at the top of this post!
Not only is this work fascinating, but it will also be useful one day. As scientists learn more about how genes and environment code for form, they envision the development of tiny living machines for medical or environmental applications – think spill clean-up in a body of water, for instance. In addition, this knowledge may eventually bring us one step closer to unlocking the hidden potential within our own cells (if possible, that is) to induce limb regeneration.
For a phenomenal, in-depth review of this paper PLUS previous publications out of this lab, check out Philip Ball’s article in Quanta.
The planarian single-step fate model
Traditional, hierarchical views of stem cell differentiation are being challenged this month.
A new study in Cell Stem Cell has proposed a model wherein stem cells are able to jump from one state to another without first entering into a phase involving fate-restricting cell divisions. They’ve called this phenomenon the “one-step fate model.”
For example, a neoblast that will eventually yield skin or intestine would also be capable of producing fate-switching cells. These wouldn’t necessarily be restricted to skin or intestine only; instead, they would be capable of producing different cell types than that which they came from.
These new findings may help us understand how planarians are such effective regenerators, thus potentially informing human regenerative medicine efforts.
Additional recommendations
April was a fantastic month in research. Here are some papers/headlines that I didn’t have room for above:
Chronological versus biological aging: Neural stem cells found to age rapidly. Ibrayeva et al. in Cell Stem Cell
Stem cell therapy being investigated for treatment-resistant bipolar disorder – clinical trial begins. University of Texas news.
Phase II clinical trial begins for Parkinson’s disease mesenchymal stem cell therapy. University of Texas news.
Visualizing neural stem cell activation via dynamic imaging, and more. Dray et al. in Cell Stem Cell.
Treating non-healing diabetic foot ulcers with stem cell therapy. Carstens et al. in STEM CELLS Translational Medicine.
Trump’s restrictions on research involving fetal tissue reversed by the NIH. Nidhi Subbaraman in Nature.
New York State kills NYSTEM, state-level funding program for stem cell research. Sofia Moutinho in Science.
hiPSC-derived glial enriched progenitor cells show therapeutic potential in white matter stroke models. Llorente et al. in Science.
Stay tuned for my next post, coming up in May!






Comments