“Regenerative medicine news under the microscope” is a monthly feature highlighting big stories in stem cell research. I will sample the latest and greatest findings in recent press and package them into a single post.
It seems that I say this every month, but wow. September was brimming with fantastic research news. In this edition, I cover the latest in our pursuit of true tissue regeneration, in vivo heart repair, an improved approach to healing degenerative disc disease, and much more!
Pick of the Month
Tissue regeneration may not be a stretch: Blocking mechanotransduction enhances wound healing and regeneration
The achievement of scar-less tissue regeneration has been referred to as the holy grail of biomedical research – it’s that critical. In human tissue, healing is achieved through fibrosis and scar formation, not regeneration. Paradoxically, this can adversely affect the organ – take a heart attack, for instance. The subsequent formation of scar tissue on the heart can lead to congestive heart failure and arrhythmias, both potentially deadly conditions. Other examples include liver cirrhosis and fibrosis of the lungs. Taken together, fibrosis costs us billions of health-care dollars each year and can cause lifelong disabilities, furthering economic impact.
As large mammals, our tissues have evolved to accommodate significant mechanical forces associated with our size. If we look at human skin, it withstands significant mechanical stress as we move, and has adapted by employing hypertrophic healing responses that result in the formation of scar tissue that’s essentially dysfunctional, characterized by a thicker dermis, increased stiffness, an absence of features like hair follicles and intradermal adipose tissue. Pigs are similar to us in this sense, so Chen et al. studied porcine wound healing responses in this important Nature Communications paper.
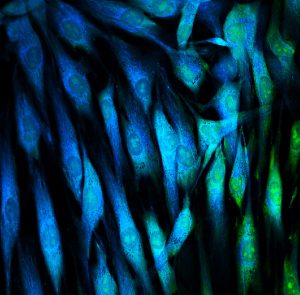
After inhibiting focal adhesion kinase (FAK), a molecular force transducer, the authors were able to promote regenerative healing and, by that, I mean that they observed a restoration in biomechanical properties of the skin, re-growth of hair follicles, and normal collagen architecture. They also aimed to confirm their findings in human tissue by studying 3D cultured human fibroblasts at the transcriptomic level, finding that FAK can pull fibroblasts away from fibrotic transcriptional states and activate regenerative phenotypes.
Interestingly, pharmacological FAK inhibition has been shown to be safe in clinical trials for cancer treatment, so there’s real promise here for the future of regenerative medicine.
A new hope for intervertebral disc disease
Between the bones of your spine lie shock-absorbing, fibro-cartilaginous discs that keep the spine flexible and are designed to resist strong forces on different axis of motion. Degenerative disc disease (DDD), though less a disease and more a condition, occurs when the spinal discs begin to break down. Unfortunately, it is one of the leading causes of disability worldwide. Though these discs show wear with age in everyone, some of us will accumulate more damage than others, causing pain ranging from mild to disabling. Progressive wear can also lead to complications like a herniated or bulging disc.
Treatment options for DDD include nonsurgical and surgical interventions, including cell-based therapies that have shown promise. Of special interest here is the injection of mesenchymal stem cell-derived chondrocytes, which are responsible for cartilage formation. However, there have been some limitations to this treatment, including hypertrophy of the differentiated chondrocytes, resulting in undesirable outcomes including apoptosis (cell death), abnormal formation, and extracellular matrix calcification. Such complications may lead to graft failure and, ultimately, unsuccessful tissue regeneration.
Bello et al. aimed to advance this promising therapy by developing a way to circumvent negative outcomes. They incorporated gelatin microparticles that were co-loaded with matrilin 3 and transforming growth factor beta 3 into mesenchymal cell spheroids (3D cell clusters or aggregates). This promoted differentiation to chondrocytes while simultaneously preventing hypertrophy. This strategy also induced the release of cytokines that promoted regeneration in vitro. The intervention worked in vivo as well, promoting regeneration of the disc tissue in rodent models.
Healing broken hearts with reversible reprogramming to a fetal state in vivo
Following injury, heart tissue regeneration is often limited. This is because the adult human heart hasn’t been found to harbour cardiac stem cells, and cardiomyocyte replacement is slow. The fetal heart, on the other hand, can regenerate. This is thanks to its immature, proliferative cardiomyocytes.
By expressing four factors (Oct4, Sox2, Klf4, and c-Myc) in a temporally-controlled, short-term de-differentiation and reprogramming protocol published in Science, Chen et al. were able to send mature cardiomyocytes back to a fetal-like state where re-entry into mitosis was possible, facilitating regeneration without initiating tumour formation.
The authors do caution that extended expression of OSKM results in tumour formation, and so the intervention must be transient to be safe. Paul Knoepfler’s take is that in vivo reprogramming protocols like this (as you may know, we’ve seen similar research in the past; see this recent paper, and this review) are a bit too risky for humans, now and likely in the future. I’ll be monitoring progress in this field for safety improvements.
High antibody responses following mRNA vaccination against COVID-19 in allogeneic hematopoietic stem cell transplant recipients
Allogeneic hematopoietic stem cell transplantation is the process by which a patient is given healthy, blood-forming stem cells sourced from a donor. This is necessary when the patient’s own cells have been destroyed due to cancer treatments or otherwise require replacement due to diseases like aplastic anemia, SCID, or sickle cell anemia. Though it’s a life-saving treatment, it does result in post-transplant immune deficiencies. The question then becomes, could COVID-19 vaccines be protective for these patients? Could an adequate immune response be generated?
Two studies have been released from two different groups with similar reporting on this question. In one study, following two doses of the BNT162b2 (Pfizer-BioNTech) vaccine, 83 per cent of patients were found to have developed an antibody response. The other group found that 76 per cent of patients developed a response to two doses of the mRNA vaccines tested (they looked at both Pfizer and Moderna and found no significant differences).
Both were relatively small studies (117 and 63 participants, respectively), thus validation on a larger scale will be required before definitive clinical guidance will be set.
A gene-editing strategy to enhance cancer immunotherapy
In recent years, scientists have been enlisting the help of the body’s own defenses in our fight against cancer. This involves activating the immune system in specific ways to enhance detection and destruction of tumours.
Our immune cells, under regular circumstances, naturally target and eliminate abnormal cells, often preventing or slowing the growth of cancer. However, cancer cells that make it past the immune system’s defenses usually harbour mutations that allow them to remain “invisible” to our immune cells, disable our immune cells, or change the healthy cells in the surrounding environment so that they interfere with the immune response to the cancer. This is where immunotherapy comes in: Clinicians arm our systems with ways to overcome the obstacles cancer cells put in place. See this helpful documentation from the NIH for details.
Woan et al. reported this month a strategy that involves the editing of induced pluripotent stem cells (iPSCs) to affect three specific changes, and the subsequent differentiation of these iPSCs to natural killer (NK) cells (a component of our innate immune system that gets involved in both anti-tumour responses and the fight against microbial infections). This made for adaptive natural killer cells mirroring those activated following invasion by cytomegaloviruses, a type of virus that stays in the human body until death. The edited NK cells persisted in vivo even without the administration of exogenous cytokines, and were found to engage in superior anti-tumour activity compared to their non-edited counterparts. They call them iADAPT NK cells and suggest that this is proof we can model specialized function of the immune system using iPSCs and deploy these new tools in the treatment of advanced cancers.
Additional recommendations
Here are some papers/headlines that I didn’t have room for above:
Induction of dopaminergic neurons for neuronal subtype-specific modeling of psychiatric disease risk. Powell et al. in Molecular Psychiatry.
Diet-induced alteration of intestinal stem cell function underlies obesity and prediabetes in mice. Aliluev et al. in Nature Metabolism.
A CRISPR/Cas9 genetically engineered organoid biobank reveals essential host factors for coronaviruses. Beumer et al. in Nature Communications.
Microvessels support engraftment and functionality of human islets and hESC-derived pancreatic progenitors in diabetes models. Aghazadeh et al. in Cell Stem Cell.
Multi-species single-cell transcriptomic analysis of ocular compartment regulons. Gautam et al. in Nature Communications.
Assessment of the structural and functional characteristics of human mesenchymal stem cells associated with a prolonged exposure of morphine. Carano et al. in Scientific Reports.
Isolation of neural stem and oligodendrocyte progenitor cells from the brain of live rats. McClenahan et al. in Stem Cell Reports.
Visualization of individual cell division history in complex tissues using iCOUNT. Denoth-Lippuner et al. in Cell Stem Cell.
Robust neuronal differentiation of human iPSC-derived neural progenitor cells cultured on densely-spaced spiky silicon nanowire arrays. Harberts et al. in Scientific Reports.
Identification of rare, transient post-mitotic cell states that are induced by injury and required for whole-body regeneration in Schmidtea mediterranea. Benham-Pyle et al. in Nature Cell Biology.
Reprogramming reactive glia into interneurons reduces chronic seizure activity in a mouse model of mesial temporal lobe epilepsy. Lentini et al. in Cell Stem Cell.
Programmatic introduction of parenchymal cell types into blood vessel organoids. Dailamy et al. in Stem Cell Reports.
Insertion/deletion and microsatellite alteration profiles in induced pluripotent stem cells. Kamimura et al. in Stem Cell Reports.
Ameliorating the hallmarks of cellular senescence in skeletal muscle myogenic progenitors in vitro and in vivo. Shahini et al. in Science Advances.
Chromatin remodeling due to degradation of citrate carrier impairs osteogenesis of aged mesenchymal stem cells. Pouikli et al. in Nature Aging.
Antiviral treatment causes a unique mutational signature in cancers of transplantation recipients. de Kanter et al. in Cell Stem Cell.
Reconstructing aspects of human embryogenesis with pluripotent stem cells. Sozen et al. in Nature Communications.
A scaffold-free approach to cartilage tissue generation using human embryonic stem cells. Griffith et al. in Scientific Reports.
Brick Strex: a robust device built of LEGO bricks for mechanical manipulation of cells. Mäntylä and Ihalainen in Scientific Reports.
Therapeutic targeting of the PLK1-PRC1-axis triggers cell death in genomically silent childhood cancer. Li et al. in Nature Communications.
Stay tuned for my next post, coming up in October!






Comments