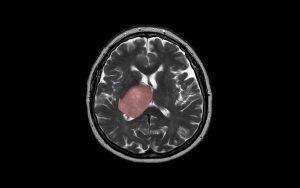
Glioblastoma multiforme – MRTT2 ax landscape “patient brain scan with glioblastoma shown in red.” Creative Commons.
In 2015, Jason Moffat walked into Sheila Singh’s office at McMaster University and gave her a small vial of clear liquid. The vial contained ten milliliters, or two teaspoons, of an injectable antibody, created in Moffat’s lab in Toronto, with a street value of around $100,000. “You better be careful with that,” Singh remembers Moffat telling her at the time.
The antibody was created to recognize and bind CD133, an antigen found on the cells that give rise to glioblastoma, an aggressive form of brain cancer with a dismal prognosis. Moffat and Singh realized they could employ the antibody to selectively target aggressive cells in brain tumours and potentially destroy them.
It raised hopes of a treatment for a disease that has, over the last few decades, seen hardly any improvement in patient survival, which stands at around 18 months post diagnosis. Glioblastoma spreads rapidly into essential brain areas making surgery difficult, while the blood brain barrier impedes the delivery of chemotherapy drugs.
Fast-forward to present time and Moffat and Singh are close to having the treatment they developed tested in glioblastoma patients. In 2018 they founded a company, Empirica Therapeutics, to translate their discoveries. CCRM provided expertise in regulatory affairs to aid successful liaisons with Health Canada, and in finance and investing to build financial models and attract other investors. One of those early investors was the Toronto-based Centre for Commercialization of Antibodies and Biologics.
According to a proof-of-principle report, published recently in the journal Cell Stem Cell, the treatment destroyed all human CD133+ glioblastoma initiating cells in the mouse brain. And an accompanying toxicity study established the approach to be generally safe with short-lived anemia as a side effect.
In June, Empirica was acquired by a U.S. stem cell company, Century Therapeutics, with patient trials for a CD133-targeting immunotherapy expected to launch as early as 2022.
Road to therapy
Moffat and Singh complement each other well as collaborators. As a professor of molecular genetics at the University of Toronto’s Donnelly Centre for Cellular and Biomolecular research, Moffat is an expert in gene editing technologies, genetics and functional genomics. Singh splits her time between running a lab at the Stem Cell and Cancer Research Institute at McMaster University and performing neurosurgery on children at the adjoining hospital and knows first-hand the devastating consequences disease and injury can leave on the brain.
Singh’s interest in glioblastoma goes back to the late 1990s when she discovered the stem cells responsible for making the tumours while doing her PhD with Peter Dirks, now Senior Scientist and Head of Neurosurgery at the Hospital for Sick Children in Toronto.
At the time, the idea of cancer stem cells, as rogue stem cells that over-proliferate into cancer instead of producing healthy cells for tissue maintenance, was beginning to gain traction. It was first proposed by John Dick, Senior Scientist at the Princess Margaret Cancer Centre in Toronto, who discovered leukemia-initiating cells and encouraged Singh to look for the equivalent cell in the brain.
In 2004, Singh published a paper showing that CD133+ cells isolated from patients’ biopsies could spawn similar tumours in mice, as the first report of cancer-initiating cells in the brain.
Moffat, who studies gene interaction networks in cancer, was interested in the molecular functions of CD133 and needed an antibody to study it. Antibodies are useful research tools because they bind tightly to their antigens and can be used to shut them down as well as label the antigen-expressing cells. Moffat’s team was able to produce a high-quality antibody against CD133 using phage display, a state-of-the-art protein engineering platform.
The researchers then harnessed the antibody for three different approaches against glioblastoma, as described in the Cell Stem Cell paper.
To target human glioblastoma, they seeded mice with human tumour cells, taken from patient biopsies. Such humanized animals allow researchers to study human tissue in a more natural setting than a Petri dish.
They first tried injecting the antibody directly into the tumours to see if shutting down CD133 could stifle their growth. The tumours shrank in size by half, but they soon grew back because the antibody only slowed down the self-renewal of CD133+ cells without killing them.
They next tried a killing approach known as dual antigen targeting engager, or DATE, also delivered by intracranial injection. Here, the antibody is engineered to pull a CD133+ cancer cell together with a cytotoxic T cell which then destroys it.
Tumours shrank again, but the DATEs turned out to be short-lived, with a half-life of 30 minutes. This would necessitate repeated drug injections, which in the brain would be impractical.
Finally, they developed an approach where a part of the CD133 antibody is engineered into the T cells, which are then injected directly into the brain or intravenously. Once released, the T cells act like homing missiles that search and destroy the CD133+ cancer cells. This form of treatment is known as CAR-T, for chimeric antigen receptor T cell, and has been successful for some blood cancers.
The treatment consisted of injecting about one million CAR-T cells once a week over a two-week period. The researchers then harvested the brains of treated and control animals, separated the cancer cells from the rest of the mouse brain cells, and counted them using a flow cytometer instrument. The human cancer cells were engineered to glow green, which enabled their sorting from host mouse cells.
Cell counts revealed that CAR-T eliminated all CD133+ glioblastoma cells, reducing the tumour size by 90 per cent. The remaining 10 percent of the cells survived because they were CD133- and could not be targeted by the treatment. The researchers are now investigating if they can devise an additional CAR-T to target the leftover tumour cells, Singh said.
Importantly, the treatment was able to reach the cancerous cells that spread from the central tumour mass to other parts of the brain, unlike the other two approaches whose effects were more localized.
The researchers worried that CAR-T might harm the healthy stem cells, which are also CD133+, and that this would affect blood production in the hematopoietic system and other stem cell-powered processes. To check for toxicity in the human hematopoietic system, they gave CAR-T to mice whose bone marrow was populated with human stem cells. They found that the stem cell pool decreased in response to the treatment, but that the effect was short lived and that the cells were able to recover between doses. Singh said that this indicates that a patient might have anemia as a result of treatment, but probably will not suffer toxicity beyond that.
As Century Therapeutics prepares for clinical trials, the therapy will look different in one key aspect: the cancer-killing T cells will not be derived from each individual patient, as is the case with the CAR-T therapies that have been approved so far. The company is developing its own allogeneic T cells engineered to avoid immune rejection as a one-size-fits-all cell product that can be given to many patients. These off-the-shelf T cells have yet to be fully tested in patients, but the ensuing therapy should be cheaper and more accessible in the long run.
Jovana Drinjakovic
Latest posts by Jovana Drinjakovic (see all)
- Canadian immunotherapy holds promise for patients with brain cancer - September 9, 2020
- Could stem cells be enlisted to battle COVID-19? - March 26, 2020
- Study reveals large differences at the molecular level between stem cells grown on different biomaterials - April 18, 2019






Comments