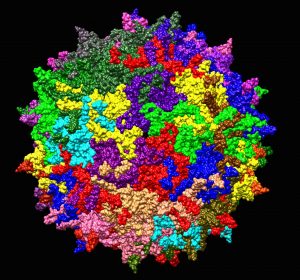
Adeno-associated virus is being used in gene therapy to shuttle healthy genes into the body. Credit: WikiMediaCommons
Plagued by failures of early human studies from the 1990s, including the death of a patient, gene therapy is making a comeback with promising results. And it has a tiny virus to thank.
After the first 2012 European gene therapy approval for a liver disease, and last year’s first U.S. approval of a therapy for blindness, a revamped gene therapy could become a long-term fix for a host of incurable illnesses. With headline-grabbing reports of stunning patient improvement from ongoing clinical trials — from haemophiliacs no longer reliant on blood clotting medication, to children able to walk after receiving the treatment for a disorder that causes paralysis and early death — we may be on the cusp of a new era in medicine in which the roots of previously incurable genetic disorders can be mended.
Based on positive results from ongoing human studies, the U.S. Food and Drug Administration announced in May it would allow a fast track approval for gene therapy for haemophilia, signalling that other diseases might follow to bring the promising new treatments to patients faster.
For all its simplicity as a concept—a disease caused by a broken gene should be fixed by putting a corrected version of that gene into the body — turning gene therapy into reality has been much harder. The problem has always been in delivery: unlike with most available drugs, which are small molecules, genes are large chunks of DNA that don’t easily get inside cells.
Today’s breakthroughs are the result of thousands of researchers who have worked over the past three decades to create weakened viruses and engineer them into gene delivery tools. Gene therapies for more than two dozen monogenic disorders – those which are caused by faults in single genes – are being tested in patients across the developed world.
In most trials, doctors are dosing patients with hundreds of trillions of particles of adeno-associated virus, or AAV, engineered to carry genes into diverse parts of the body without causing any harm in itself. This makes the AAV-based gene therapy a far cry from the first wave of human studies that relied on adenoviruses and retroviruses that were less safe but were easier to grow and engineer at the time. (The AAV was initially isolated with the adenovirus and remains linked to it in name, although the two viruses are very different.)
Jesse Gelsinger
An infection with the adenovirus, even when it is stripped of its viral replication genes and stocked with a healthy human gene, provokes an immune response that can be lethal. This was the case in the 1999 trial, in which Jesse Gelsinger, an 18-year-old clinical trial volunteer, tragically died. Gelsinger’s death brought an end to human studies that lasted almost a decade, eroding public trust and leaving researchers scrambling for dwindling research funding while trying to develop safer viruses. As one gene therapy pioneer recently said to The Guardian, ”The reputation of gene therapy went from being a cure for all known diseases to something you wouldn’t give your dog.”
At the same time, early attempts to deliver healthy genes using retroviruses were plagued by the virus’ tendency to jump randomly into the host cell genome, potentially disrupting gene function in a way that could spur cancer. This is what happened to several children who developed leukemia after receiving treatment for an immune disorder in a French trial from 2000.
AAV does not have these problems: it does not stir up the immune system and it deposits its gene cargo as a separate piece of DNA beside the host cell genome. The AAV can also infect cells in various parts of the body – muscles, liver, even in the brain – thanks to its ability to cross the blood-brain barrier, a formidable obstacle for many drugs. The AAV’s main caveat is its limited cargo capacity, which means it can only carry small and medium-sized genes. Also, it’s not very good at infecting immune cells. For immune disorders, researchers are testing lentiviruses to deliver genes into immune cells in the dish before transplanting them into patients.
Attesting to AAV’s safety are more than 1,000 patients—an estimate given to me by Luk Vandenberghe, a gene therapy researcher at Harvard University—who have so far received AAV-based gene therapy in various trials over the years with no ill effects.
Going forward
Last year saw the start of a new trial for Ornithine transcarbamylase (OTC) deficiency, the disease that Jesse Gelsinger had. The disease causes ammonia, the by-product of liver protein metabolism, to build up to dangerous levels in the blood, which can cause coma and death.
“Jesse Gelsinger permeates the whole discussion about gene therapy in OTC,” says Dr. George Diaz, Chief of the Division of Medical Genetics at Mount Sinai’s Icahn School of Medicine in New York and one of the investigators on the new OTC trial, adding that it was very important to do the trial safely.
“The safety profile of AAV is really what drove the decision-making. Adenoviral vectors clearly had problems with inflammatory reactions that were seen in the bodies of patients exposed to these vectors,” says Dr. Diaz. “AAV does not have that.”
The first AAV was isolated just over 50 years ago. Since then, virologists have uncovered hundreds of AAV variants, each slightly different from one another and in their ability to target different tissues. The new OTC trial is using a variant called AAV8, which easily enters liver cells, making it well suited for the treatment of liver defects.
Another variant, AAV5, has transformed the lives of haemophiliac patients. First isolated in the 1980s, from a man’s genital wart of all places, the AAV5 is a telling, if unappealing, example of how progress in medicine often comes from unexpected places. Researchers are also designing new synthetic AAV variants to further improve delivery that should make gene therapy applicable to more disorders.
As remarkable as the current progress in the field is, gene therapy won’t work for every genetic disorder. In its current form, it can only target diseases that start to unfold after birth, while developmental disorders beginning in the womb remain out of reach. Also, current trials target only a sliver of the 7,000 or so monogenic disorders which are rare and affect a small number of people. For 3,000 of those, we don’t even know what are the genes that cause them. The decision to develop a therapy will depend on which part of the body is affected and when, the gene size, but also the size of the patient population so that drug makers can turn a profit.
Hurdles remain, but for swathes of trial volunteers whose suffering has been reduced thanks to gene therapy, life is already much better. That’s something to celebrate.
Jovana Drinjakovic
Latest posts by Jovana Drinjakovic (see all)
- Canadian immunotherapy holds promise for patients with brain cancer - September 9, 2020
- Could stem cells be enlisted to battle COVID-19? - March 26, 2020
- Study reveals large differences at the molecular level between stem cells grown on different biomaterials - April 18, 2019






Comments