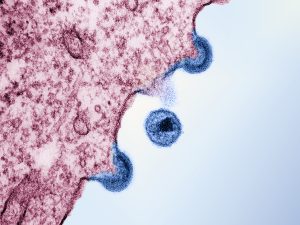
HIV-1 viral particles (blue) budding from an infected cell in vitro. Transmission electron micrograph captured at the National Institute of Allergy and Infectious Diseases Integrated Research Facility. Credit: NIAID.
Pick of the Month
Another HIV-1 remission, but with a twist: The Geneva Patient
I previously wrote about Mr. Paul Edmonds, who was the fifth person in history to be cured of both HIV-1 and leukemia since the first such case in 2009. This was achieved through a hematopoietic stem cell (HSC) transplant and, according to experts, the key to success was a donor mutation conferring HIV-1 immunity: CCR5-Δ32/Δ32.
We now have data indicating that this genetic rarity, present in just 2 per cent of the population, may not be necessary to achieve remission in every transplant case. Romuald, a 53-year-old man now widely referred to as “The Geneva Patient,” appears to have achieved long-term remission of his HIV following an HSC transplant from a donor without the CCR5 mutation. Incredibly, we don’t currently know how this is possible, as other patients have received wild-type transplants in previous years and were not cured.
Part of the reason why we don’t yet understand this phenomenon is that Romuald’s medical history was complex, lengthening the list of possible contributing factors. For instance, he suffered through several episodes of graft-versus-host disease. Could the episodes themselves – or the treatments to get them under control – have played a role in Romuald’s remission? We’ll have to wait for these answers.
The circumstances surrounding Romuald’s transplant are also highly serendipitous. The only reason he received wild-type cells was that a CCR5-Δ32/Δ32 donor was unavailable at the time of his care, which was in 2018. Technically, the second person to be cured via the CCR5-Δ32/Δ32 mutation hadn’t been reported until 2019 (ten years after the first case!) so this was rather new territory. His doctors went ahead with the procedure anyway, and the rest is now cemented in medical history.
Now I will admit, the data was originally published in September; however, given the magnitude of the results, I wanted to monitor expert responses first. Indeed, new commentary was published this month in Nature, offering up the perfect opportunity for discussion in the current edition.
It appears a new chapter of HIV-1 research has officially begun.
A nasal spray for Alzheimer’s disease?
Imagine a nasal spray that could delay the progression of Alzheimer’s disease (AD) by up to 15 years.
We’re not quite there yet, of course, but new research out this November has demonstrated the possibility in preclinical models.
Microglia and astrocytes – referred to as glial cells – are essential to brain function. They maintain the blood-brain barrier, provide synaptic support, and are also key players in immune function. When stimulated to do so, these cell types are capable of clearing out AD-related plaques, but they concurrently produce inflammation that can be harmful to neurons. That being said, this functional state of activation, or reactivity, ultimately perpetuates AD pathology.
To tackle this catch-22, Madhu et al. purified extracellular vesicles (EVs) from human iPSC-derived neural stem cells and administered the resultant biologic to young adult mice (approximately three months old). The purified EVs naturally contained anti-inflammatory miRNAs and proteins, which is why they were hypothesized to be beneficial in this disease context.
Examining the same mice between six weeks to two months later, they found they were able to modulate the activity of glial cells: Overall neuroinflammatory gene expression and inflammatory protein levels were reduced relative to untreated controls, as were the amount of beta-amyloid plaques. Cognitive function and mood were also improved. Thus, the treatment seems to have only prevented harmful glial overactivity, rather than non-specifically blunting performance altogether; beneficial plaque cleanup functions were spared, while damaging activity was dialled down.
The research group reported similar molecular effects in human cell culture assays.
It should be noted that 3-6 month-old mice are roughly equivalent to 20-30 year-old humans. As mentioned at the beginning of this highlight, the therapy appears to have delayed disease progression at a theorized mouse equivalent of 10-15 years (but keep in mind this is a hypothetical extrapolation). Future work should determine whether the EVs will be more effective as a preventative treatment, or if they might also ameliorate disease outcomes if administered in older, more progressed patients.
I do wish we’d seen an experiment where they tried out their biologic with aged AD animals, but these studies require significant time and resources, so it’s quite understandable that this avenue hasn’t been investigated yet. The researchers also mention in their discussion that neurons take up the EVs as well, and that the contributions of this phenomenon to the cognitive improvements they observed have yet to be determined. Furthermore, modulation of the immune system, especially in the brain, is not a trivial undertaking. Clinical trials will be very important in determining potential side effects and, of course, we don’t know if the effects will carry over to humans. Regardless, the implications of the study make it a highly interesting read.
There are currently unrelated, FDA-approved drugs designed to slow down AD. However, these have been quite controversial; if you’re interested, see this Medical News Today article for context. It discusses the recent meta-analysis by the American Academy of Family Physicians on the topic.
All eyes on Japan: iPSCs take on limbic stem cell deficiency
You might recall Johanne Provost’s story, which I covered in the September edition of RMNU🔬. Ms. Provost had been fighting a rare autoimmune disorder that induced fibrosis over her cornea, obscuring her vision. She received a limbal stem cell transplant sourced from a deceased donor, and two years later, her vision was restored. While this procedure was a success, Ms. Provost will have to remain on immunosuppressive medications. The ultimate goal of transplant medicine is to remove this stipulation, and work published last month may have brought us one step closer to this goal.
Dr. Kohji Nishida’s team at Osaka University published the results of a small trial to ascertain the safety of an iPSC-based treatment for limbal stem cell deficiencies, such as the one suffered by Ms. Provost. A critical factor in the Osaka study, however, was that the iPSCs were not generated from the patients themselves. The intention was to develop an allogeneic therapy, where donor blood cells were reprogrammed and differentiated into a sheet of corneal epithelium that would ultimately replace the patient’s scarred ocular tissue. The reason why – along with the trade-off – matters greatly in this context. That’s why I wrote a full-form blog on this, so watch out for it in early January!
While there are efforts ongoing to reduce or eliminate the immunogenic properties of “off-the-shelf” iPSC therapies, the authors further argue that their specific disease case offers unique advantages in this regard. Previous experiments have shown lab-grown corneal epithelial cell sheets to have limited immunogenicity as assayed in cynomolgus monkeys. Just in case, the trial was designed such that two of the four patients were on corticosteroids, and the other two were administered corticosteroids plus low-dose cyclosporine (an immunosuppressive drug). Two years post-treatment, none of the four patients presented with severe side effects such as tumour formation. Critically, patients did not appear to be entirely immunotolerant of the cells; indeed, there was no overt rejection, but the immunosuppressed group exhibited more pronounced visual improvements. It seems that subclinical immune rejection may have been a factor in the corticosteroid-only group.
A much larger trial, beginning in March, is being organized to determine efficacy. For now, the data collected thus far do afford a preview: All four patients experienced immediate vision improvements; however, one individual’s particularly severe underlying condition is thought to have caused a regression of their improvement to baseline.
If the next trial is successful, it may pave the way for either autologous or engineered, virtually non-immunogenic allogeneic iPSC treatments in future. For now, the Osaka strategy may still mark an improvement as compared to the current benchmark, since rejection rates are quite high (40 per cent, according to the authors) following standard corneal limbal transplants, such as those from cadavers.
First to the line: Brain-injectable gene therapy wins fast-track FDA approval
Serotonin and Dopamine are two of the most recognizable neurotransmitters in the brain thanks to their involvement in multiple well-known diseases and, by extension, their frequent references in pop culture. On the other hand, aromatic L-amino acid decarboxylase (AADC) – a critical enzyme involved in the synthesis of these two heavy-hitting molecules – is discussed less in the mainstream. Under ultra-rare genetic circumstances (<1 per 50,000 people), individuals can’t produce sufficient amounts of the protein, a heritable condition referred to as AADC deficiency.
While disease severity may be highly variable from case to case, AADC deficiency can profoundly affect neurological growth, leading to developmental delays, intellectual disabilities, and movement disorders. The involuntary (autonomic) nervous system may be impacted as well, causing issues with blood pressure, body temperature, pupillary constriction, heart rhythms, and more. Overall, these patients tend to be at very high risk of death in the first 10 years of their lives.
PTC Therapeutics has developed a gene therapy, called Kebilidi, which is administered to patients in a single surgical session. A recombinant adeno-associated virus (rAAV2, specifically) containing copies of the functional human gene coding for the enzyme is injected directly into the putamen, the same region targeted in recent Parkinson’s disease stem cell trials – see my coverage of those in the 2024 May and summer editions. Patients receive two infusions of the gene in the anterior part of the putamen, and two in the posterior part. The injections are meant to boost dopamine production, aiming to ameliorate movement-related symptoms.
Kebilidi just received fast-track approval from the FDA as a result of positive data from an ongoing clinical trial; safety and efficacy were preliminarily demonstrated in a small, early-stage cohort of 13 afflicted children with no gross motor function, but who appeared to show improvements 48 weeks post-injection. That makes Kebilidi the first ever brain-injectable gene therapy to be approved by the FDA. The accelerated approval pathway is reserved for therapies treating severe or fatal conditions, and is granted only upon evidence that a product is reasonably likely to be of clinical benefit. Longer-term follow-up studies of their trial participants will be required, in addition to further proof of efficacy. There are possible side effects of both the drug and surgery, ranging from sleeping problems to strokes.
It will be interesting to see whether future therapies will also attempt to boost serotonin production via strategic delivery of the gene to a serotonin-focused brain structure. For now, there’s already precedent for movement targets, so boosting dopamine in the putamen seems like a well-established place to start.
Additional recommendations
Sexual dysfunction and suicidal thoughts – the dark side of anti-balding drugs. You might want to send this article to those in your circle who might be taking finasteride, also known as Propecia from Organon, or Avodart by GSK. This news was also covered by Medscape last month, as the European Medicines Agency is currently investigating.
Sickle cell patient dies in Beam study of base editing therapy. This death was reportedly caused by busulfan, a chemotherapy agent also used with Casgevy and Lyfgenia. Ned Pagliarulo put it really well in his piece for BioPharma Dive linked above: “The patient’s death highlights the challenges developers like Beam face in advancing cutting-edge gene editing techniques that still require the blunt tools of decades past.”
FDA probes blood cancer risk from bluebird’s gene therapy, weighs regulatory action. The original FDA announcement can be found here. There’s also a piece with more detail about this issue at Nature Biotechnology: Cancer cases in bluebird’s gene therapy trials.
Therapeutic potential and mechanisms of stem cells in major depressive disorder: a comprehensive review. Although I don’t usually include many reviews, this one is conceptually intriguing.
Adult skull bone marrow is an expanding and resilient haematopoietic reservoir. Such interesting findings here, especially for those who follow ageing research: “Furthermore, skull is largely protected against major hallmarks of ageing, including upregulation of pro-inflammatory cytokines, adipogenesis and loss of vascular integrity.”
Deciphering influence of donor age on adipose-derived stem cells: in vitro paracrine function and angiogenic potential. This study is somewhat surprising as they find that donor age is not necessarily a factor in their study population: “Our results show cells from young and old donors exhibit no difference in all assessed parameters, suggesting all patients could be included in clinical applications. We emphasized the leading role of ASC in angiogenesis, without impairment with age, where secretome is a key but not sufficient actor.” Other papers have linked ageing to decreases in stem cell performance; this one from October is an example, as is this one from 2017. Perhaps it depends on the type of stem cell.
The emergence of Sox and POU transcription factors predates the origins of animal stem cells. This paper is only loosely related to regenerative medicine, given the transcription factors and the involvement of iPSCs – but I couldn’t resist. It’s an absolutely fascinating practical demonstration of the reason why we use other creatures to study ourselves: the genetic similarities are astounding. This is a must-read.
Extracellular vesicles derived from endothelial progenitor cells modified by Houshiheisan promote angiogenesis and attenuate cerebral ischemic injury via miR-126/PIK3R2. If you’re interested in Traditional Chinese Medicine, this one may be for you.
GIOSTAR Announces FDA Clearance of the IND for Starting PHASE-2 Clinical Trial for Developing Specific Stem Cell Therapy for Type II Diabetes. Yet another player is emerging in the diabetes RM arena.
Two potential drugs that could improve gene therapy for sickle cell disease: More stem cells for sickle cell gene therapy readied with motixafortide, and Cyclosporin H boosts uptake of gene therapy in SCD newborn stem cells.
CRISPR Clinical Trial Targets Sickle Cell at Its Genetic Roots. This strategy involves direct gene editing to target the disease mutation, rather than an edit that compensates for the defect caused by the original mutation (the route taken by current FDA-approved options).
A pair of urine-derived stem cell papers: Efficient generation of human induced pluripotent stem cells from urine samples of patients with Fragile X syndrome, and Direct conversion of urine-derived cells into functional motor neuron-like cells by defined transcription factors.
CRISPR Nobelists surrender their own European patents. Imagine having to surrender a patent because it’s not detailed enough, even if you’re Doudna and Charpentier.
Bone Marrow Donors Can Be Hard to Find. One Company Is Turning to Cadavers. Not necessarily unprecedented, given the limbic stem cell story mentioned above!
Intravenous and intracranial GD2-CAR T cells for H3K27M+ diffuse midline gliomas.
The Human Cell Atlas: towards a first draft atlas.
Hope Biosciences’ stem cell therapy shows promise in small Phase 2 trial.
Achieving myoblast engraftment into intact skeletal muscle via extracellular matrix.
What’s the secret to living to 100? Centenarian stem cells could offer clues.
A comprehensive human embryo reference tool using single-cell RNA-sequencing data.
Largest ALS patient-based stem cell, biodata resource opens for research.
Biocooperative Regenerative Materials by Harnessing Blood-Clotting and Peptide Self-Assembly.
Early-stage trial finds stem cell therapy for retinitis pigmentosa is safe.
mTOR activity paces human blastocyst stage developmental progression.
Control of spatio-temporal patterning via cell growth in a multicellular synthetic gene circuit.
This scientist treated her own cancer with viruses she grew in the lab.
Cell tumbling enhances stem cell differentiation in hydrogels via nuclear mechanotransduction.
Patient iPSC models reveal glia-intrinsic phenotypes in multiple sclerosis.
Mapping aged stem cell states associated with decline in skeletal muscle regeneration.
Regulated GATA1 expression as a universal gene therapy for Diamond-Blackfan anemia.
Capricor seeks FDA approval of deramiocel for Duchenne based on encouraging data.






Wow, this was such an informative and well-explained update! I really enjoyed how you made complex topics easy to understand. Great job summarizing everything so clearly!
Lyla does a great job. I’m glad you are enjoying her regular posts on regenerative medicine advances making the news.