The volume of clinical updates I encounter every month is steadily but very noticeably growing month over month! There are lots to get through, so in this rapid-fire edition of RMNU🔬, you’ll find short summaries on all the biggest headlines of the summer’s first half.
Pick of the Summer (so far)
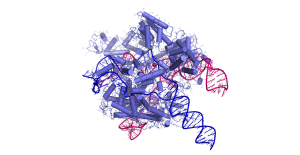
The first custom CRISPR therapy
Six months, one week, and four days. That’s how long it took scientists to create a custom CRISPR therapy for baby KJ, who was suffering from a rare, life-threatening condition called CPS1 deficiency – short for carbamoyl phosphate synthetase I deficiency. That’s unprecedented, given how long drug development usually takes: 10+ years based on what I’ve seen in the healthtech investment space.
CPS1 deficiency is a genetic defect of the process by which the body metabolizes protein. What results is a buildup of ammonia in the tissue, which can be toxic (especially in the brain). Estimated to have an infant mortality rate of 50 per cent and affect just 1 in 1,300,000 people, even if the child survives, there’s still a risk of developmental delays and intellectual disabilities.
Of course, once the baby is diagnosed, their protein consumption is often significantly restricted and nitrogen scavenging medication is usually prescribed. In KJ’s case, rather than the usual liver transplant that would follow, the research team of Musunuru et al. developed a custom CRISPR therapeutic to edit the infant’s genetic code. To date, KJ has been stable and is consuming more protein and less medication, suggesting efficacy. However, longer follow-up will be required to assess the overall safety and determine just how well the treatment works. So far, so good, however! Read more in this NIH news release.
Lots of movement on the Parkinson’s front
I’ve been tracking all of the biggest progress on cell therapies for Parkinson’s across editions of RMNU🔬 – check out the spring edition for a summary table I put together.
Aspen Neuroscience, approaching the problem using induced pluripotent stem cell (iPSC)-derived dopamine neuron progenitors, just published six-month data from their first three patients in the ASPIRO Phase I/IIa trial. As is the case with trials from other groups, early data are hinting at both safety and efficacy. Check out their press release here.
From the same team that brought us the STEM-PD trial (also covered in the spring edition) comes data from the TransEuro trial attempting human fetal ventral mesencephalic transplantation in patients with Parkinson’s. This study kicked off in 2010 and, overall, the primary endpoint was not met. The team does appear to have learned a lot from this trial, however, as things are expected to go much better with STEM-PD.
Lastly, I think we all get quite excited when a drug that’s already been approved by the U.S. Food and Drug Administration (FDA) for one thing proves to be effective within another indication. There are entire labs dedicated to identifying these multi-tool drugs. It seems we could have another one on our hands: an antibody used to treat melanoma (nivolumab/relatlimab) is showing preclinical promise, though a lot of work remains. This article has a nice summary of the work if you’d like to learn more.
Vertex’s diabetes cell therapy: Zimislecel data published
In the last edition, I discussed Vertex’s decision to drop VX-264 – their device-encapsulated pancreatic islet cell therapy. Now, the group has published their data on VX-880 (now called Zimislecel), the unencapsulated version of their therapy that requires immunosuppressants. Their findings can be summarized in the following quote:
“Ten of the 12 participants (83%) had insulin independence and were not using exogenous insulin at day 365.”
That’s impressive. It should be noted, however, that two patients in the trial died; one from cryptococcal meningitis following a seemingly unrelated surgery, but that was deemed to have resulted from immunosuppression, and the other from dementia-related causes. The former case is, of course, especially disappointing, and is yet another practical example of why teams are pushing so hard for cell therapies that do not require immunosuppressants.
As previously mentioned, as a result of these generally positive results, their Phase I/II trial was upgraded to Phase I/II/III. Enrollment and dosing for approximately 50 patients are slated to wrap in the first half of 2025. For more details, I’d really recommend this piece over at Medscape.
Placenta-derived mesenchymal stem cells deemed safe in multiple sclerosis patients
Mesenchymal stem cells (MSCs) from donated placentas were well tolerated by five individuals with secondary progressive multiple sclerosis (MS) in a small Phase I trial, a more advanced stage of the disease.
The patients first received chemotherapy to rid them of their existing, diseased immune cells. Placental stem cells are then infused into the body to regenerate the immune system so that it’s less likely to attack nerve cells. The process is intended to reduce MS symptoms and slow disease progression. We have early hints at efficacy in this trial, but it was too small to know for sure.
Temporary headaches appear to be the worst side effect they detected. Otherwise, nothing serious. Hopefully, they move into Phase II and we get more data soon.
ALS updates
The FDA has cleared a Phase IIIb trial for NurOwn, an autologous, bone marrow-derived MSC cell therapy developed by BrainStorm. This follows the conclusion of their Phase III trial, which apparently did not meet their primary endpoint. However, in a smaller subgroup analysis of patients with less advanced disease, results showed more promise. Biomarker data also supported the drug’s continued study, with fewer markers of nerve damage detected in the spinal fluid. This story is highly similar to that of another biotech company from South Korea – CorestemChemon – and their Neuronata-R MSC therapy.
The way the cells are manufactured is supposed to be highly specific, such that they secrete higher levels of neurotrophic factors and immunomodulatory cytokines – all to say, they’re meant to modulate neuroinflammation while promoting neuroprotection.
This new study will enroll 200 participants.
Also check out this ALS paper in Cell Stem Cell: An organ-chip model of sporadic ALS using iPSC-derived spinal cord motor neurons and an integrated blood-brain-like barrier.
In vivo CAR T-cell therapy and more
As you likely know, CAR T-cell therapies available in clinics are currently ex vivo: T cells are removed from the body, upgraded in the lab, then returned to the patient. Taking this strategy to the next level, researchers have been working on a way to upgrade T cells without removing them first. A very cool example of this was published by Hunter et al. last month. Their team developed an in vivo genetic engineering strategy to reset the immune system and create CAR T cells in humanized mice and cynomolgus monkeys. They use targeted lipid nanoparticles to deliver the mRNA to specific subsets of T cells.
Also, check out this great news piece in Nature Reviews Drug Discovery that does a good job of summarizing progress in this space.
Bonus: A Gilead-backed CAR T-cell therapy shrank recurrent glioblastoma tumours in 62 per cent of patients. They use two molecular targets since solid tumours are often heterogeneous. Sadly, the benefit appeared to be temporary as many patients relapsed two to three months later. The team is now working on a version of the therapy with three targets to see if they can do better.
Cancer vaccines could be on the horizon
Phase I enrollment in a clinical trial for Anixa Biosciences’ breast cancer vaccine just wrapped up. It’s a set of three shots given two weeks apart. So far, 35 women have received the vaccine:
- 26 of them have completed treatment for triple negative breast cancer (that’s the most aggressive form, so they’re cancer-free, but at risk of recurrence);
- Four fall into a category for “prevention” (they have risky mutations and are opting for a preventative mastectomy); and,
- Five are post-operative and receiving a cancer immunotherapy drug called pembrolizumab.
The vaccine targets alpha-lactalbumin, a milk protein. Apart from lactation, it is typically not found in healthy breast tissue. It is, however, expressed in about 70 per cent of triple-negative breast cancer cases.
We could see safety data as early as the fall of this year, but preliminary results suggest that the vaccine is well-tolerated and that it does indeed mobilize an immune response. Phase II is currently being planned.
A pancreatic cancer vaccine is also in preclinical development; see the June news release on this.
Additional recommendations
Remembering James Till, a pioneer in stem cell research.
Failed stem cell transplant contributed to death. This is an alarming story out of the UK – the 2024 death was entirely preventable, caused solely by a lack of appropriate testing on both the donor and the recipient. It seems understaffing and capacity issues are being blamed.
FDA Announces Investigation of Deaths Following Treatment With Sarepta’s DMD Gene Therapy Elevidys. In the Spring Edition of RMNU🔬, I included a brief note on the first death. A second death has been linked to the gene therapy, also due to acute liver failure, and so the FDA is officially investigating. It is important to note that over 800 patients have received the product across real-world and clinical trial settings, but the risks are still very real. Also, the two patients who passed were nonambulatory, and so it seems the research team is looking into modifying the treatment regimen for this demographic specifically. Their Phase III clinical trial is now on hold.
First Stem Cell Medicine Course for Clinicians Available for Free. It’s not just for clinicians! It’s open access and available to everyone. This is what their page says: “For clinicians, medical students, scientists, and the public.” There’s no reason not to register and go through the materials!
A single factor for safer cellular rejuvenation. It’s not normal to publish a “scientific” paper about a gene, but then keep that gene hidden. I understand that the team is treating it as a trade secret for business reasons, but asking for blind trust at any stage is unreasonable, especially in the wake of other controversies. I doubt the paper will get accepted into a mainstream journal as-is for this reason. It’s especially strange as a strategy because this is what patents are for. If the team can produce an intervention to manipulate the gene, they can file a patent like any other biotech company. Seems like they’re intentionally trying to spur speculation/discussion/suspense.
STEMCELL Technologies Announces Acquisition of Cellular Highways. I usually wouldn’t comment on acquisitions as part of RMNU🔬, however, products from STEMCELL Technologies can probably be found inside every biomedical research building in my city (Toronto, Canada). I figured a new technology in their portfolio might be of interest.
CRISPR used to remove extra chromosomes in Down syndrome and restore cell function. This is a great read on a paper that came out this past February: Trisomic rescue via allele-specific multiple chromosome cleavage using CRISPR-Cas9 in trisomy 21 cells.
Regeneration Biomedical’s Cell Therapy Reduces Tau, Boosts Cognition in Alzheimer’s Cases. I will discuss these data when their peer-reviewed publication is available, so stay tuned!
In vivo haemopoietic stem cell gene therapy enabled by postnatal trafficking. Plus a thematically related story, Ensoma Announces FDA Clearance of IND Application for First In Vivo HSC-Directed Gene Insertion Therapy.
Senescence and inflammation are unintended adverse consequences of CRISPR-Cas9/AAV6-mediated gene editing in hematopoietic stem cells. Nobody wants to fix one thing by breaking another. This paper does offer up a solution to the problem, so that’s positive.
And finally, so much human clinical trial progress that I didn’t even get the chance to highlight all the progress in vascularizing organoids:
- Engineered vasculature induces functional maturation of pluripotent stem cell-derived islet organoids.
- Self-organization of sinusoidal vessels in pluripotent stem cell-derived human liver bud organoids.
- Rapid generation of functional vascular organoids via simultaneous transcription factor activation of endothelial and mural lineages.
Don’t rush promising stem-cell therapies.
Engrafted nitrergic neurons derived from hPSCs improve gut dysmotility in mice.
Tiny human hearts grown in pig embryos for the first time.
Harnessing human iPSC-microglia for CNS-wide delivery of disease-modifying proteins.
Outcomes of Allogeneic Hematopoietic Stem Cell Transplant in Monogenic Inflammatory Bowel Disease.
NHS plans to DNA test all babies to assess disease risk.
Metabolic adaptations direct cell fate during tissue regeneration.
CRISPR-based screening pinpoints H2AZ1 as a driver of senescence in human mesenchymal stem cells.
Creatine monohydrate pilot in Alzheimer’s: Feasibility, brain creatine, and cognition.
Graft-versus-Host Disease Prophylaxis with Cyclophosphamide and Cyclosporin.
Clonal tracing with somatic epimutations reveals dynamics of blood ageing.
Post-gastrulation amnioids as a stem cell-derived model of human extra-embryonic development.
FXYD2 marks and regulates maturity of β cells via ion channel-mediated signal transduction.
The biggest questions facing regenerative medicine.
Notable global approvals and status changes
EMA Conditionally Authorizes Stem Cell Therapy for Blood Cancers.






Comments