Elisa D’Arcangelo holds a PhD in Biomedical Engineering from the University of Toronto. She is working as a Postdoctoral Fellow at the Princess Margaret Cancer Centre, using tissue engineering and organoid approaches to understand the lung cancer microenvironment and its role in tumour recurrence. Other science pursuits include making perfect ravioli and imperfect pottery.
The escalating spread of the SARS-Cov2 virus has been a public reality since the beginning of 2020. Research into the infection dynamics of coronaviruses, however, far pre-dates this timeline – coronaviruses were identified in the mid-1960s – highlighting not only the fact that every novel virus represents a challenge for research, but also that, by now, virologists can draw on a well-established arsenal of techniques to figure out the virus’ biology. This includes infecting panels of target cells with a virus of interest.
The cells used in this approach are usually not freshly sourced from a donor (human or other animal); instead they have been grown in labs for many years and thus no longer resemble their tissue counterparts. (An extreme example of this are HeLa cells, the first human cells ever to be successfully grown outside of the body, which were isolated from tissue in 1951.) And even if the cells have been recently isolated from tissue, the stress of conventional cell culture methods selects for only the heartiest of them, thus ensuring that cultures quickly drift towards being homogeneous and lacking the variety initially observed. Ongoing clinical trials for candidate vaccine compounds against SARS-Cov-2 are all based on initial findings made using these cells.
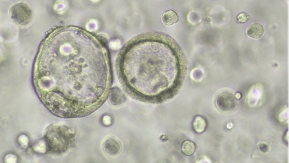
Recently, a new method to perform cell culture has been developed and may prove to be a powerful addition to the virologist’s repertoire of techniques. This method generates organoids – three-dimensional structures that self-assemble in a dish – starting from embryonic or adult stem cells, which are sourced from a donor.
These mini-organs resemble their tissue counterparts, meaning they contain the correct variety of cells and arrange into the morphologies observed in the actual tissue. They are young, non-homogeneous and complex cell cultures, all of which are advantages scientists are now hoping to leverage to study novel virus biology.
The first study using organoids for virus work was published only a few years ago; it allowed researchers to observe host-norovirus interaction where there was previously no robust way to culture the virus within living cells. Since then, organoids have been used to study a number of viral diseases, including congenital anomalies due to Zika infection and the effects of influenza viruses, including the H1N1 virus responsible for the 2009 pandemic.
Today, PubMed reports dozens of studies, carried out in the last few months, specifically on the use of organoids for SARS-Cov-2 research. These have been asking some crucial questions, including: what tissue and what cells are the virus’ target? And what can be done to stop infection or to improve clinical outcome?
Capitalizing on the fact that organoids contain multiple cell types, a team in Japan has unveiled that SARS-CoV-2 preferentially infects organoid cells with stem-like properties, suggesting that it is the adult stem cell population that replenishes other lung cell types, which is the primary target of the virus.
Another study in airway organoids showed how the virus induces cells to produce specific molecules that have been observed in patients during so-called cytokine storms (a hyper-inflammatory state that inflicts great damage and can ultimately be fatal). Organoids formed from diverse tissues have also clarified how the virus could make its way from the lung into other sites in the body, including gut, brain, pancreas, kidney and liver; by reaching the cells lining blood vessels in the lung, SARS-Cov-2 may gain access to the whole body via the circulatory system.
While these studies are fundamentally concerned with understanding the multi-faceted consequences of SARS-Cov-2 infection, they do beg the question as to what the organoid technology has contributed towards vaccine development. The answer is, not much.
While researchers speculate that organoids can be used as tools for drug discovery or to test the efficacy of drugs in suppressing viral infection, the major question emerging at the crossroads of the organoid and vaccine development fields is: How complex is too complex?
The aspects that play in favour of organoids when it comes to studying fundamental biology also render them rather impractical models for drug development and testing. Higher complexity comes at the price of scalability and homogeneity. Organoids are comparatively expensive to culture and their production cannot be scaled up quite like that of the cheaper, more homogeneous cell lines.
Most importantly, however, and specifically because organoids are not homogeneous cell populations, their response to infection is more complex to decipher. Currently, no head-to-head comparison has been done between the utility of organoids and cell lines for the discovery of new targets or therapeutic candidates. Until such studies are done extensively, cell lines will remain at the forefront of screening efforts, precisely because they are less complex.
Guest
Latest posts by Guest (see all)
- Regenerative immunotherapy: Hope for chronic autoimmune diseases - September 16, 2025
- Canada’s regenerative revolution: Why AI is the catalyst - September 4, 2025
- Summer by Design: A launchpad for future entrepreneurs and industry scientists - August 14, 2025






Comments